As we rapidly approach the point where the Covid-19 vaccine is available to all those who want it, the key constraint on reaching a sufficiently high level of vaccinations to achieve herd immunity is the hesitancy of certain groups to get vaccinated. The latest survey data from the Kaiser Family Foundation breaks them down. As one can see in the first chart, 10 percent of Black adults refuse to get vaccinated—which, fortunately, is down from 27 percent in October 2020—with 7 percent saying they will only get vaccinated if forced to and another 24 percent reporting a wait-and-see attitude. Although a higher percentage of whites say they will refuse a Covid vaccination outright, a third fewer will get one only if required or take a wait-and-see position.
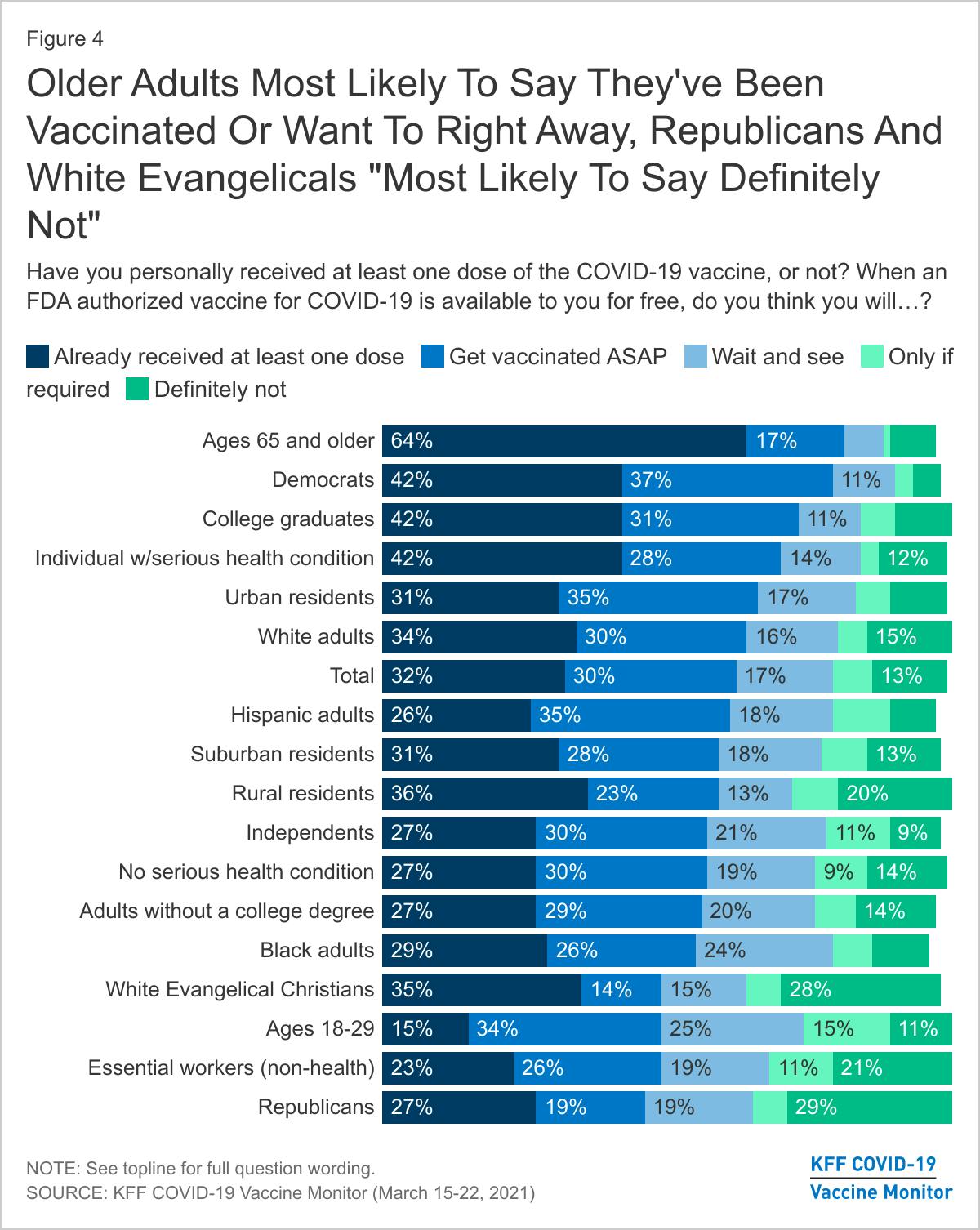
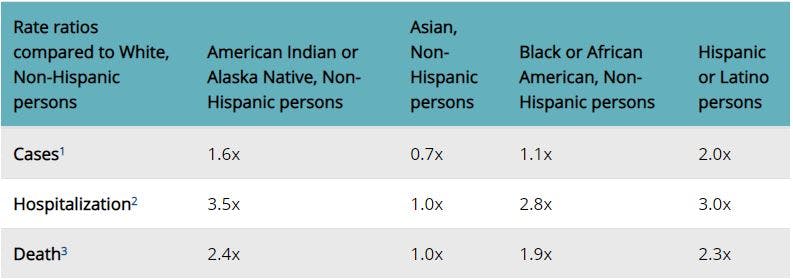
While much attention has focused on crazy conspiracy theories that cause Republicans to resist getting vaccinated, it is disturbing that a large percentage of Black adults remain skeptical of doing so, as well, despite this group having a death rate from Covid-19 almost twice, and a hospitalization rate almost three times, that of the non-Hispanic white population, according to the Centers for Disease Control and Prevention (second chart). And these data likely understate the true death toll among Blacks caused by Covid-19 by at least 10 percent, according to a recent study in the Journal of Racial and Ethnic Health Disparities, based on the death rate from all causes.
None of this is happening in a vacuum. A February 2021 study in the journal Clinical Infectious Diseases found that the historical maltreatment and mistreatment of Black people by the medical establishment is an important reason why so many are skeptical of the Covid-19 vaccine. At least one participant in the study specifically mentioned the Tuskegee syphilis experiment as a reason to resist getting vaccinated.
Vaccine hesitancy among Blacks is nothing new. They have long been less likely to get the seasonal flu vaccine than whites. They have also been reluctant to participate in HIV vaccine trials, despite a higher incidence of the disease among African Americans, according to the CDC. In 2018, 39.2 percent of all those diagnosed with HIV were Black, though they compose just 13.4 percent of the U.S. population. Again, the Tuskegee legacy is often cited as a reason for this reluctance.
The Tuskegee syphilis experiment is the most notorious in the history of medicine. It is summarized on the CDC website as follows:
In 1932, the Public Health Service, working with the Tuskegee Institute, began a study to record the natural history of syphilis in hopes of justifying treatment programs for blacks. It was called the “Tuskegee Study of Untreated Syphilis in the Negro Male.”
The study initially involved 600 black men—399 with syphilis, 201 who did not have the disease. The study was conducted without the benefit of patients’ informed consent. Researchers told the men they were being treated for “bad blood,” a local term used to describe several ailments, including syphilis, anemia, and fatigue. In truth, they did not receive the proper treatment needed to cure their illness. In exchange for taking part in the study, the men received free medical exams, free meals, and burial insurance. Although originally projected to last 6 months, the study actually went on for 40 years.
The study only ended because its existence was revealed by the Associated Press in 1972. At the time the study commenced there was no cure for syphilis, which was a serious and widespread problem. During World War I, it was the second-most-common reason for soldiers to be disabled. However, while the purpose of the original study may have had some justification, it took a seriously perverse turn in the 1940s when it was discovered that syphilis could be cured by penicillin. By the late 1940s, penicillin was widely available yet was never offered to participants in the Tuskegee study, which continued until 1972. At the time its existence was revealed, at least seven men had died directly from syphilis and 74 of the original participants still survived.
On October 1, 2010, it was revealed that from 1946 to 1948, the U.S. government conducted a second study of syphilis in Guatemala, where 700 prison inmates, mental patients, and soldiers were intentionally infected. As The New York Times reported:
American tax dollars, through the National Institutes of Health, even paid for syphilis-infected prostitutes to sleep with prisoners, since Guatemalan prisons allowed such visits. When the prostitutes did not succeed in infecting the men, some prisoners had the bacteria poured onto scrapes made on their penises, faces or arms, and in some cases it was injected by spinal puncture.
At least in the Guatemala study, the victims were treated with penicillin, since its purpose was to gauge the effectiveness of the treatment. (Those in the Tuskegee study acquired syphilis on their own and, contrary to popular belief, weren’t intentionally infected; they just weren’t treated properly. In both cases, however, the studies failed to get informed consent from participants.) The same day that details of the Guatemala experiment were revealed, Secretary of State Hillary Clinton and Department of Health and Human Services Secretary Kathleen Sebelius offered an apology to the victims. President Barack Obama phoned the president of Guatemala to express regrets. (The original report that revealed the existence of the Guatemala study was done by Wellesley historian Susan Reverby and published in the Journal of Policy History in 2011.)
It should be noted that biological ethics were quite different in those days. For example, Dr. Tom Rivers, often called the “father of modern virology,” admitted in a posthumously published oral history that in the early 1930s he personally tested a yellow fever vaccine on patients without their permission and, contrary to law, failed to disclose to the public in New York City that there were cases of yellow fever in their midst. (See page 187 in Tom Rivers—Reflections on a Life in Medicine and Science, published in 1967.)
In 1973, 40 survivors of the Tuskegee experiment filed suit in federal court seeking damages for their treatment. The following year, survivors who were syphilitic were each granted $37,500 (about $200,000 today), and nonsyphilitic survivors received $15,000 (about $80,000 today). Estates of the former got $15,000, and those of the latter got $5,000. Ultimately, $9 million was paid out to some 6,000 heirs. The last participant died in 2004. The Trump administration opposed further payouts in 2017. Neither survivors nor estates of the Guatemala experiment received any payments at all.
In 1996, Tuskegee University established a Syphilis Study Legacy Committee, which issued a report in May of that year. It noted that the syphilis experiment continued to “cast a long shadow over the relationship between African Americans and the biomedical professions.” It urged President Clinton to issue an official apology for those who suffered, which he did on May 16, 1997. Said Clinton, “The United States Government did something that was wrong, deeply, profoundly, morally wrong. It was an outrage to our commitment to integrity and equality for all our citizens.”
A number of studies have shown that the revelation of the Tuskegee experiment had a long-term effect on the willingness of African Americans to go to doctors and hospitals and to be vaccinated, with profound effects on the health of the Black community. The latest study of this effect by the economists Marcella Alsan and Marianne Wanamaker came to this startling conclusion:
We find that the disclosure of the [Tuskegee syphilis] study in 1972 is correlated with increases in medical mistrust and mortality and decreases in both outpatient and inpatient physician interactions for older black men. Our estimates imply life expectancy at age 45 for black men fell by up to 1.5 years in response to the disclosure, accounting for approximately 35% of the 1980 life expectancy gap between black and white men and 25% of the gap between black men and women.
Personally, I am less certain that the Tuskegee study caused African Americans to shun doctors, hospitals, and biomedical research so much as it symbolized—very clearly and indisputably—aspects of the health system that were long viewed as being racist in effect if not intent. One study of the Tuskegee experiment concluded that “Tuskegee is not a central event in the African American ethos; instead for some, the Tuskegee study represents another example of why the medical system cannot be trusted.”
The legacy of Tuskegee is probably just one factor in the reluctance of some Black people to get vaccinated for Covid-19. More prosaic factors include the unavailability of transportation to vaccination sites and lack of internet access to schedule appointments. However, the legacy of racism in the health system cannot be ignored, which is why the Biden administration has launched an initiative to address the problem. It’s a start.








